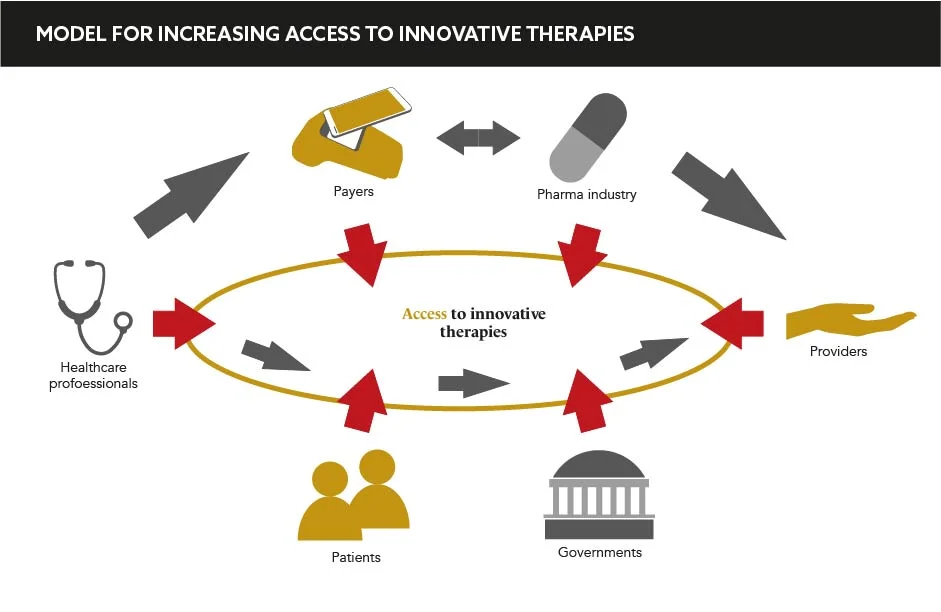
The pandemic has exacerbated already troubling trends in the market access but has also created an opportunity for change. The industry must collaborate with governments to increase the adoption of innovative therapies for the benefit of patients all over the world
Words by Isabel O’Brien
The price of a pint of milk fluctuates as economies thrive and falter, but the cost of pharmaceuticals is less tied to economic disparities or downturns. As a commodity, a drug must be treated differently to a pint of milk, but as pressures on healthcare systems intensify due to COVID-19, how can the pharma industry establish checkout solutions that enable the most innovative treatments to be adopted by all healthcare systems, rather than just by a privileged few?
While the pricing debate has been raging in the background for decades, it had reached particularly dizzying heights in the months leading up to the pandemic. Trends such as an increase in ageing populations and a rise in chronic diseases led to the affordability of drugs being placed under the microscope. Speaking at ‘Reuters Events: Pharma 2021’, Sylvie Greneche, Head of Global Market Access, General Medicines, Sanofi, explains: “In the pre-COVID period, there were already many trends in market access that we were dealing with.” While the pandemic has provoked transformation across most facets of healthcare, pricing is one area where the issues have remained the same, or even worsened. “The pandemic has accelerated price pressures, and the trends have not changed,” Greneche adds. This is illustrated by the recent experience of Bluebird Bio, which failed to reach agreements with European healthcare systems for its blood disorder treatment Zynteglo due to the $1.8mn price tag. The industry is at turning point for market access – but how can it pivot and drive impactful change?
It’s like turning the proverbial oil tanker
Historically, the problem has been angled predominantly at the industry, but the attitude to costly and innovative therapies by governments must be tackled if these treatments are to be considered, let alone adopted, by the world over. “There is too much focus on rewarding activity and cost containment and there is not enough focus on what the system should be doing, which is delivering health outcomes for patients,” says Greneche. While healthcare systems must be designed to serve the majority, she believes that governments are too focused on cutting their budget on innovative therapies, but actually “the proportions spent on innovative drugs is very small”. She emphasises that savings in this area are not savings at all. Martin Price, Vice President, Health Economics, Market Access and Reimbursement, Janssen, agrees. “It’s like turning the proverbial oil tanker, but that doesn’t mean that we shouldn’t focus on it,” he says.
If governments can become more flexible in their attitudes, the rigidity of treatment price tags must be next on pharma’s checklist for an overhaul. Also speaking at the Reuters event, Ulf Staginnus, Market Access Executive, details: “We must move away from having one exam or assessment, setting one price, then that’s it for the lifecycle.” The current assessment system perpetuates stagnation that is both unhelpful and outdated.
As real-world data capabilities expand, Staginnus explains that the industry must adopt living and breathing pricing structures. “We need a system where, as we learn and see data, the pricing and reimbursement system can be adapted.” While fluctuation is often perceived as negative, in this context, fluidity could be key. The same applies for the greater use of innovative pricing structures from the outset, particularly in lower-to-middle-income countries. Price recommends the concept of equity-based pricing, “where you modify the price of the medicines that you offer according to the country’s gross national income per capita”.
While these direct problems with pricing require the most urgent attention, there are other caveats that must be considered when seeking to solve troubles in market access. “It is not always price or affordability that is the barrier. Often there are non-price access barriers such as expertise, healthcare infrastructure and a lack of trained professionals to treat patients,” says Price. For many healthcare systems, even if they can afford the funding or be granted access at a reduced cost, the issue of delivering the therapies to patients still acts as a blocker.
The system is not ready, but pharma is not ready either
The issue of access to innovative treatments is complex, but the outcome if they are not resolved is clear. Staginnus says: “These trends will have to be addressed. Otherwise, we may see polarisation in some markets and further delays in others that are more pronounced than ever before.” Just as a price of a pint of milk can rise and fall, the industry must create greater flexibility in its approach to pricing. “The system is not ready, but pharma is not ready either,” concludes Greneche. The industry must work with governments to build superior pricing structures fit for the future, which will ensure no therapy is left on the shelf.