Throughout the pandemic, frontline workers valiantly managed patient care amidst disruptions and strains on healthcare systems across the globe. While this attention was channelled to COVID-19, however, patients awaiting other treatments were deprioritised. How can pharma ensure no patients are left behind?
Words by Michaila Byrne
If at any point during lockdown you were forced to cut your own hair, bake your own bread, or host your own Zoom quiz, you have probably, to some extent, bought into a newfound ‘do it yourself’ attitude.
This is of course, a best-case scenario if you are fortunate and privileged enough to be in a comfortable environment; nevertheless, this mentality shift has been adopted the world over, allowing us to discover hobbies and realise skills we never knew we possessed.
However, when it comes to patient care, a ‘can-do attitude’ can only go so far; at some point, it is time to see the doctor. As the pharmaceutical and healthcare industries near ever closer to combatting COVID-19, how can we ensure that non-COVID-19 patients are re-prioritised and encouraged to seek the care they need?
Putting patients first
If there’s one thing that needs to be outsourced, it is obtaining an expert opinion from a medical professional. As a result of social distancing, capacity challenges, and infection protocols, common routes for detection have been on pause.
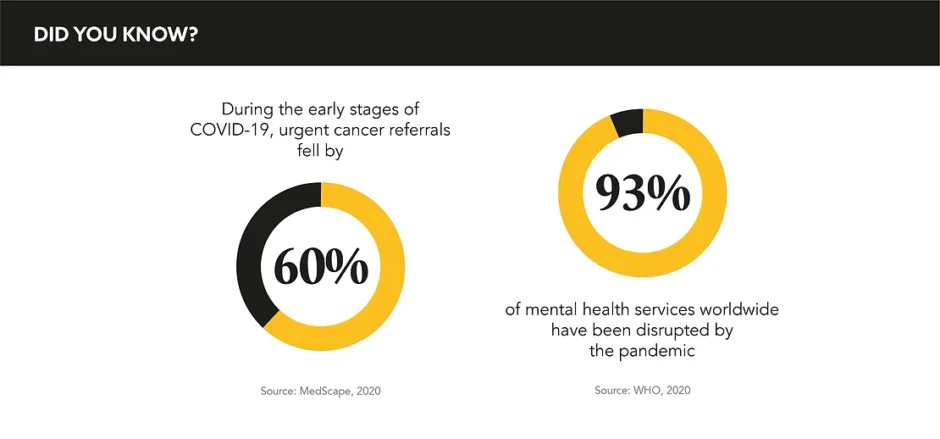
“All patient populations have been negatively impacted in some way, be it by delays in diagnosis due to postponed appointments, missed treatments due to fear of visiting the doctor, or from a psychological point of view,” outlines Steffen Kurzawa, Head of Global Communications and Member of the Executive Committee, Sandoz. Such disruptive changes in the environment can risk the start of a domino effect, negatively impacting patient emotional well-being from both a social and economic perspective.
Kurzawa also highlights another long-term implication that is at present unclear: “the impact of antibiotic prescriptions given to COVID-19 patients for potential secondary infections on patterns of antimicrobial resistance.”
Disruptions in patient care
This knock-on effect is particularly glaring in oncology, as David Long, Business Unit Director, Oncology, MSD confirms: “Some of the common routes for cancer detection – like national screening programmes and routine dental appointments which pick up head and neck cancers – paused altogether for a period in 2020.”
Other areas facing major upheaval are complex diseases such as multiple sclerosis and other autoimmune disorders, where delays now can trigger a vicious cycle of health problems. Valerie Amies, Founding Director, The Marle Partnership, expresses that: “My concern is about the impact on services during the recovery phase, which is probably the next 5-10 years at least.”
Naturally, with internal resources all hands-on deck for the pandemic, delays in getting new drugs approved for medicines unrelated to COVID-19 are to be expected. “All of the efforts for new drug approvals have been reallocated to vaccines, and rightfully so, but this could have long-term implications for innovation and progression of medicines hitting the market,” says Amanda Demarzo, Associate Director, Patient Access, ACMA, calling the impact on non-COVID-19 patients “astronomical.”
Taking health online
In the meantime, the industry has adapted to not having the use of brick-and-mortar locations for healthcare by embracing the power of digital alternatives, namely telemedicine.
“The usage of telemedicine is having a positive impact on the workload in the hospitals during the pandemic; this may help patients to connect with their HCPs now and in the future. However, telemedicine also has its limitations, and it has to be integrated smartly and appropriately into the patient treatment journey to create a lasting positive impact,” explains Kurzawa.
It is vital that time is taken to rebuild trust with patients, but in the meantime, pharma can assist in ensuring that healthcare systems are well-equipped with the essential medicines required to treat all patients.
Ramping up NHS recovery
An unforeseen challenge are those patients who have long ignored and tend to play down their need for help. The unity and collective support for the frontline workers we have witnessed has been inspiring, but it does mean that people could be less inclined to ‘bother’ HCPs and feel they are doing a service by not raising concerns or coming in.
MSD’s ‘Do It for Yourself’ campaign wants to assure patients that this is not the case: “It recognises that we have become a nation of DIY-ers during lockdown, and that people might want to prioritise their health as they would do fixing up their homes,” explains Long.
He suggests that the role for the pharmaceutical industry in the UK is in helping the NHS recover by: “Acting quickly to fill some of the gaps we see opening. For us, that was not just in promoting health-seeking behaviour, but also to provide grants to support resilience of the charitable sector and survive the hit to fundraising income they had seen.”
It has never been more vital to hammer home the message to patients that they haven’t been forgotten about and that their doctor wants to see them. To ensure that people aren’t taking Google’s opinion as gospel, the industry needs to re-engage all patients with the healthcare system, letting them know they are a priority, and that no one will be left behind.